An Overview of Parkinson’s Disease
Parkinson’s disease is a progressive neurological disorder that affects movement. It is the second most common neurodegenerative disease after Alzheimer’s disease, impacting millions of people worldwide. This blog post provides a comprehensive overview of Parkinson’s disease, covering its symptoms, diagnosis, causes, pathology, and treatment options.
What is Parkinson’s Disease?
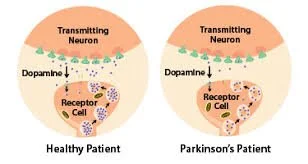
Parkinson’s disease is a chronic and progressive movement disorder. It occurs when nerve cells (neurons) in a specific area of the brain called the substantia nigra deteriorate or die. These neurons produce dopamine, a neurotransmitter that plays a critical role in sending messages to the part of the brain that controls movement and coordination. As dopamine levels decrease, it becomes harder for the brain to regulate movement and coordination.
Symptoms
Symptoms of Parkinson’s disease generally develop gradually and worsen over time.
Motor Symptoms:
Tremor: Shaking, often starting in a limb, most commonly in the hands or fingers. The tremor can be more pronounced when at rest.
Bradykinesia: Slowness of movement, making simple tasks difficult and time-consuming.
Rigidity: Stiffness and inflexibility of the limbs and trunk, which can be painful and restrict the range of motion.
Postural Instability: Impaired balance and coordination, leading to an increased risk of falls.
Non-Motor Symptoms:
Sleep Disorders: Trouble sleeping, restless legs syndrome, or REM sleep behavior disorder.
Mood Disorders: Depression, anxiety, and apathy.
Cognitive Impairment: Memory problems, difficulty concentrating, and slowed thinking.
Autonomic Dysfunction: Issues with blood pressure regulation, digestion, bladder control, and sweating.
Sensory Symptoms: Loss of sense of smell (anosmia), pain, and discomfort.
Diagnosis
Diagnosing Parkinson’s disease can be challenging because there are no specific tests for it. The diagnosis is primarily based on medical history, symptoms, and neurological examinations.
Medical History and Symptom Assessment: A detailed discussion about symptoms, medical history, and family history.
Neurological Examination: Assessing motor function, reflexes, muscle strength, coordination, and balance.
Imaging Tests: While not definitive for diagnosis, MRI or CT scans may be used to rule out other conditions that could cause similar symptoms.
DaTscan: A specialized imaging test that helps visualize dopamine transporter levels in the brain, which can support the diagnosis.
Response to Parkinson’s Medication: Improvement in symptoms after taking Parkinson’s medication, such as levodopa, can support the diagnosis.
Causes
The exact cause of Parkinson’s disease is unknown, but it is believed to result from a combination of genetic and environmental factors.
Genetics: About 15% of people with Parkinson’s have a family history of the disease. Specific genetic mutations have been linked to Parkinson’s, including mutations in the LRRK2, PARK7, PINK1, and SNCA genes.
Environmental Factors: Exposure to certain toxins, such as pesticides and herbicides, has been linked to an increased risk of Parkinson’s. Other factors include head injuries and living in rural areas.
Age: The risk of developing Parkinson’s increases with age, with most people being diagnosed after age 60.
Gender: Men are more likely to develop Parkinson’s disease than women.
Pathology
Parkinson’s disease is characterized by the progressive loss of dopamine-producing neurons in the substantia nigra, a part of the brain involved in movement control. This leads to a decrease in dopamine levels, which affects the functioning of the basal ganglia, a brain region that regulates movement.
As well, there is a presence of Lewy bodies, abnormal aggregates of protein (alpha-synuclein) inside neurons. These Lewy bodies are thought to contribute to the death of neurons and the progression of the disease.
Treatments
While there is no cure for Parkinson’s disease, treatments are available to manage symptoms and improve quality of life. Treatment options include medications, surgical interventions, and lifestyle changes.
Medications:
Levodopa: The most effective medication for Parkinson’s, levodopa is converted to dopamine in the brain, helping to manage motor symptoms.
Dopamine Agonists: Medications that mimic dopamine’s effects in the brain, such as pramipexole, ropinirole, and rotigotine.
MAO-B Inhibitors: These medications, like selegiline and rasagiline, inhibit the enzyme that breaks down dopamine, increasing dopamine levels in the brain.
COMT Inhibitors: Medications like entacapone and tolcapone that prolong the effect of levodopa by blocking its breakdown.
Amantadine: Provides short-term relief of symptoms and helps reduce dyskinesias (involuntary movements).
Surgical Interventions:
Deep Brain Stimulation (DBS): A surgical procedure that involves implanting electrodes in specific parts of the brain. These electrodes deliver electrical impulses to help regulate abnormal brain activity.
Lifestyle Changes:
Exercise: Regular physical activity can improve mobility, balance, and overall well-being.
Nutrition: A balanced diet helps maintain general health. Some people find that a high-fiber diet can alleviate constipation, a common non-motor symptom.
Therapies: Physical, occupational, and speech therapy can help manage symptoms and maintain independence.
Conclusion
Parkinson’s disease is a complex and progressive neurological disorder that significantly impacts the lives of those affected and their families. While there is no cure, understanding the symptoms, diagnosis, causes, pathology, and treatment options can help manage the disease and improve the quality of life for those living with it