Navigating Type 2 Diabetes: Insights from My Uncle’s Journey
Today I interviewed a family member with Type 2 diabetes. They have had diabetes since their twenties, and now in their fifties, they have learned to manage it. They would like to let everyone know that it is hard work to manage their diabetes, but it is worth it.
What is diabetes?
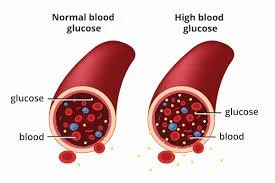
Diabetes is a metabolic and chronic disease occuring when the body either doesn't produce enough insulin or can't effectively use the insulin it produces. Insulin is a hormone made by the pancreas that allows your body to use glucose from carbohydrates in the food for energy or to store glucose for future use.
There are three main types of diabetes:
Type 1 Diabetes: An autoimmune condition where the immune system attacks insulin-producing beta cells in the pancreas. It is usually diagnosed in children and young adults.
Type 2 Diabetes: A condition where the body becomes resistant to insulin or doesn't produce enough insulin. It is more common in adults but is increasingly seen in younger populations due to rising obesity rates.
Gestational Diabetes: Diabetes that develops during pregnancy and usually goes away after giving birth. However, it increases the risk of developing type 2 diabetes later in life.
Symptoms
Symptoms of diabetes may occur suddenly. In type 2 diabetes, the symptoms can be mild and may take many years to be noticed. My family member experienced all of these symptoms.
Frequent urination (polyuria)
Excessive thirst (polydipsia)
Extreme hunger (polyphagia)
Unexplained weight loss
Fatigue
Blurred vision
Slow-healing sores or frequent infections
Tingling or numbness in hands or feet (more common in type 2 diabetes)
Diagnosis
Hemoglobin A1C: Measures your average blood glucose for the past two to three months. Diabetes is diagnosed at an A1C of greater than or equal to 6.5%
Fasting Plasma Glucose Test (FPG): Measures blood glucose levels after an overnight fast. A level of 126 mg/dL or higher indicates diabetes.
Oral Glucose Tolerance Test (OGTT): Measures blood glucose before and two hours after consuming a sugary drink. A level of 200 mg/dL or higher after two hours indicates diabetes.
Random Plasma Glucose Test: Measures blood glucose levels at any time, regardless of when you last ate. A level of 200 mg/dL or higher, along with symptoms of diabetes, indicates diabetes.
Causes
The causes of diabetes vary depending on the type:
Type 1 Diabetes
The exact cause of type 1 diabetes is unknown, but it's believed to be a combination of genetic predisposition and environmental factors, such as viruses that might trigger the autoimmune response. As well, it is thought to be caused by an autoimmune reaction, meaning, the body attacks itself by mistake. This reaction destroys the cells in the pancreas that make insulin, called beta cells. This process can go on for months or years before any symptoms appear.
Type 2 Diabetes
Type 2 diabetes is primarily influenced by lifestyle factors and genetics. Key factors include:
Insulin Resistance: The body's cells become resistant to the effects of insulin, leading to higher blood sugar levels.
Pancreatic Dysfunction: Over time, the pancreas may produce less insulin.
Genetics: Family history and certain genetic markers increase the risk.
Obesity: Excess body fat, especially around the abdomen, is a major risk factor.
Physical Inactivity: Lack of exercise contributes to obesity and insulin resistance.
Gestational Diabetes
Hormonal changes during pregnancy can lead to insulin resistance. Risk factors include obesity, a family history of diabetes, and having had gestational diabetes in a previous pregnancy.
Treatments
The treatment of diabetes aims to manage blood sugar levels and prevent complications. Treatment strategies vary depending on the type of diabetes:
Type 1 Diabetes
Insulin Therapy: Daily insulin injections or the use of an insulin pump to maintain blood sugar levels.
Blood Sugar Monitoring: Regular monitoring of blood glucose levels using a glucometer or continuous glucose monitor (CGM).
Diet and Exercise: A balanced diet and regular physical activity to maintain a healthy weight and control blood sugar levels.
Type 2 Diabetes
Lifestyle Modifications: A healthy diet, regular exercise, and weight loss are crucial in managing type 2 diabetes.
Oral Medications: Medications like metformin help lower blood sugar levels by improving insulin sensitivity or reducing glucose production by the liver.
Insulin Therapy: Some individuals may require insulin injections if oral medications are insufficient.
Blood Sugar Monitoring: Regular monitoring to track blood sugar levels and adjust treatment as needed.
Gestational Diabetes
Lifestyle Changes: Healthy eating and regular physical activity.
Blood Sugar Monitoring: Frequent monitoring to ensure blood sugar levels remain within target ranges.
Medication: Insulin or oral medications may be prescribed if lifestyle changes are insufficient.
Conclusion
Diabetes is a complex disease with significant health implications. Understanding its causes, symptoms, diagnosis, and treatment options is crucial for effective management. With proper medical care, lifestyle adjustments, and continuous monitoring, individuals with diabetes can lead healthy and fulfilling lives. If you suspect you have diabetes or are experiencing symptoms, consult a healthcare professional for a thorough evaluation and personalized treatment plan.
My family member recommends those especially with type 2 diabetes to manage their diet, and to choose foods with a low glycemic index. He mentions he has learned to plan ahead of time in order to make the best food choices.
World Health Organization. "Diabetes."